Joash Ogwoka
Tracheomalacia, common among young children and infants, is a condition in which the supporting cartilage present in the trachea is weakened. The weaken cartilage causes the significant changes to the trachea breathing dynamics. In severe cases, this may lead life- threatening disruption of airflow. Some children with symptomatic tracheomalacia must spend long periods of time in the hospital.
A tracheotomy is a procedure in which the trachea is opened. This procedure is needed for patients in need of long -term mechanical ventilation and those with upper airway obstruction, copious secretions and weaning failure. Early-hemorrhage, infection, subcutaneous emphysema, tube obstruction-and late-swallowing problems, tracheal stenosis, tracheo-innominate artery fistula etc.-complications may result after a tracheotomy.
In the case of tracheomalacia long term data of the condition is only available through esophageal atresia studies. The extent of the symptom relationship between tracheomalacia and esophageal atresia is unclear. The paucity of data of this condition and absence of long-term data for children with indwelling airway stents warrants a method by which such data may be acquired reliably. By employing simulations, tracheomalacia may be models and the long-term effects of the condition itself and in tracheomalacia-inflicted children with indwelling airway stents may be modeled. The data acquired from successful simulation could increase knowledge about the condition and improve treatment methods and devices. Further, the effects of a tracheotomy may also be simulated by inputting patient specific parameter. This could better help predict the effects a tracheotomy and possible short- and long-term complication. It is therefore crucial to establish reliable simulations. In this study, the reliability of simulations in ANSYS was assessed. Tracheomalacia, tracheotomy and normal trachea conditions were simulated in ANSYS and compared to experimental values.
Materials:
1. Software: ANSYS
The trachea tissue properties were modeled with a thickness of 1mm, width of 10mm, elastic modulus of 20kPa and Poisson’s ratio of .3. The cartilage ring properties were modeled with a thickness of 1mm, width of 10mm, elastic modulus of 20kPa and Poisson’s ratio of .3. Tracheomalacia was simulated using 500kPa for the elastic modulus of the cartilage ring.
Engineering Data
In ANSYS, under engineering data, a new material was created and the elastic modulus and Poisson’s ratio was entered under Young’s Modulus and Poisson’s ratio. Geometry A sweep arc of 300 degrees was created. Radial lines were drawn from the center of the arc to the ends of the arcs. The arc was then closed between these two lines. 3D mode and trimetric view was employed. The edge of the large arc, i.e. cartilage ring, was selected and ‘pull’ was selected and the pull direction was set as the z-axis . A pull of 5mm was executed. ‘No merge’ was selected and a pull of 5mm was executed on the smaller arc, i.e. connective tissue. The back faces were deleted to form an open ring. Both edges of the rings were selected using ctrl-click, ‘no merge’ employed and a pull of 10mm was executed. This 10mm section was tissue was to represent the tissue between cartilage rings. The appropriate labels were made under Design1. Linear pattern was then used. All the components and the z-axis were selected. 7 and 15mm were inputted under X-count and X-pitch respectively. All of the components were selected, right clicked and selecting independent. The last 10mm tissue was then deleted. Clicking design, under Share Topology, ‘share’ was selected.
Model
A thickness for the large arc surface(1.1mm), cartilage ring small arc(1mm), connective tissue between the cartilage ring, and the 10mm ring(1mm), tissue between cartilage rings, and corresponding material was selected under Graphic Properties. A mesh was generated. Mesh, sizing was used and all the elements were selected for a total of 20 faces. The element size was set to 1.5mm. Thick Shells and Beams Style was turned off. Static Structural was right clicked, then insert, and then fixed support. Both edges on the ends of the ‘tube’ were selected and four edges were created in geometry. Static Structural was right clicked, then insert, and then pressure. The internal faces, not external, faces were selected and 20 faces were created in geometry. The pressure was set to 100Pa.
Solution
Solution was right-clicked, then insert, then Deformation and then Total. Static Structural was right clicked and then solve.
Results:
The (1.0)True Scale was selected. Total Deformation was right-clicked, then export and then stl. On the Workbench homepage, under Component Systems, geometry was selected. A The stl file was then uploaded in Geometry. After opening geometry, Facets was right-clicked, then Convert to solid and then merge faces. Under repair, missing faces was selected and the two missing faces were selected. Under measure, mass properties was selected and the solid body created was selected. The volume in mm^3 was displayed.
Tracheotomy Geometry
The above created geometry was modified as follows. Create plane was selected, then the y-axis, then move and the ring was moved +6.4mm on the y-axis. Split body was clicked, the forth cartilage rings was selected and the plane was clicked. This created split the cartilage ring into thirds. The properties of the middle third piece were changed to those of the tissue to simulate the a tracheotomy. The other two thirds were unchanged.
Ansys simulation showed that the volume decreases from the normal trachea in tracheomalacia and in a tracheotomy. The changes were much more pronounce in the case of tracheomalacia where a decrease of up to 1.16% was observed and only up to .26% in the tracheotomy. The compliance in both cases also changed. A compliance(mm^3/Pa) of 11.29, 12.67 and 11.79 was observed in the normal trachea, tracheomalacia and tracheotomy, respectively. When normalized to volume, the compliance per volume unit was .000396, .00046, .000414. for normal trachea, tracheomalacia and tracheotomy, respectively.
| Pressure(PA) | Normal Volume(mm^3) | Tracheomalacia Volume (mm^3) | Tracheotomy Volume (mm^3) |
|---|---|---|---|
| 100 | 28510 | 28404 | 28491 |
| 150 | 27912 | 27755 | 27886 |
| 200 | 27323 | 27116 | 27291 |
| 250 | 26744 | 26488 | 26707 |
| 300 | 26175 | 25871 | 26133 |
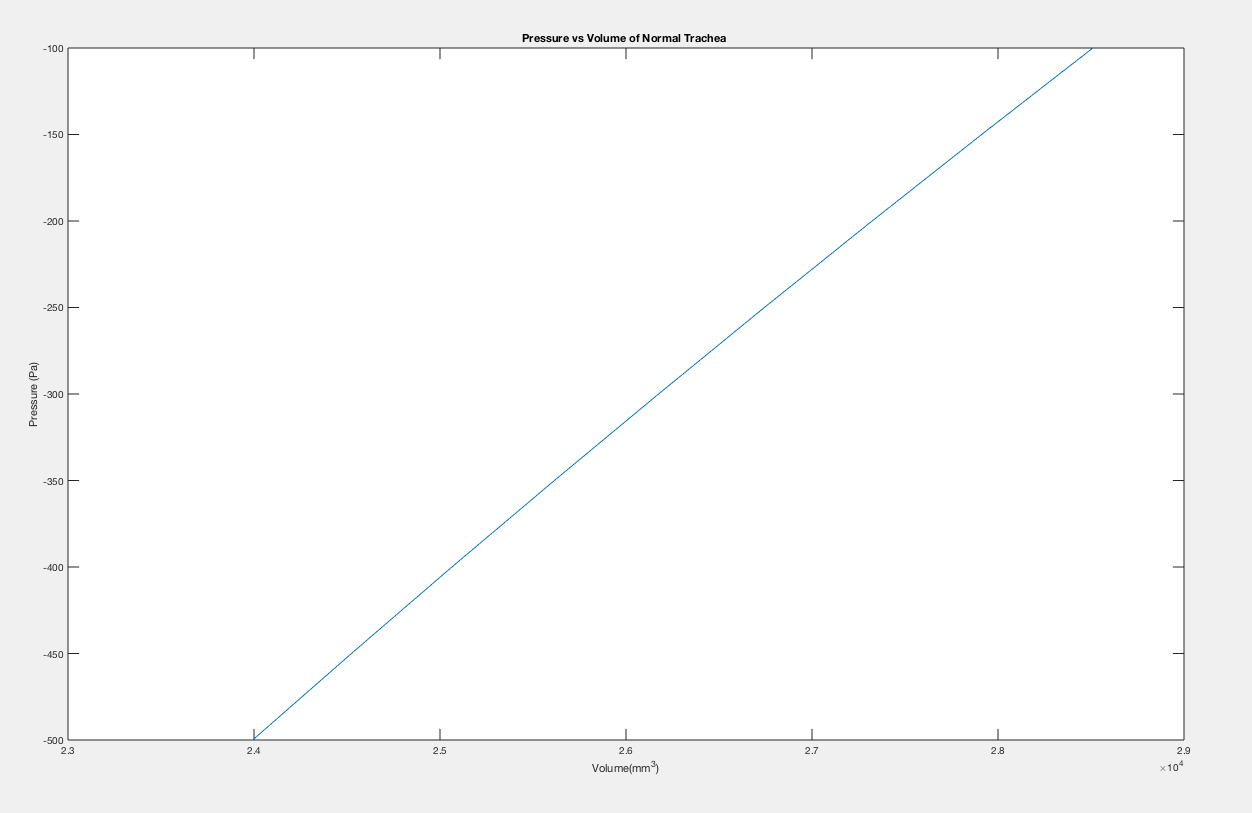
Figure 1:
Pressure vs Volume of Normal Trachea
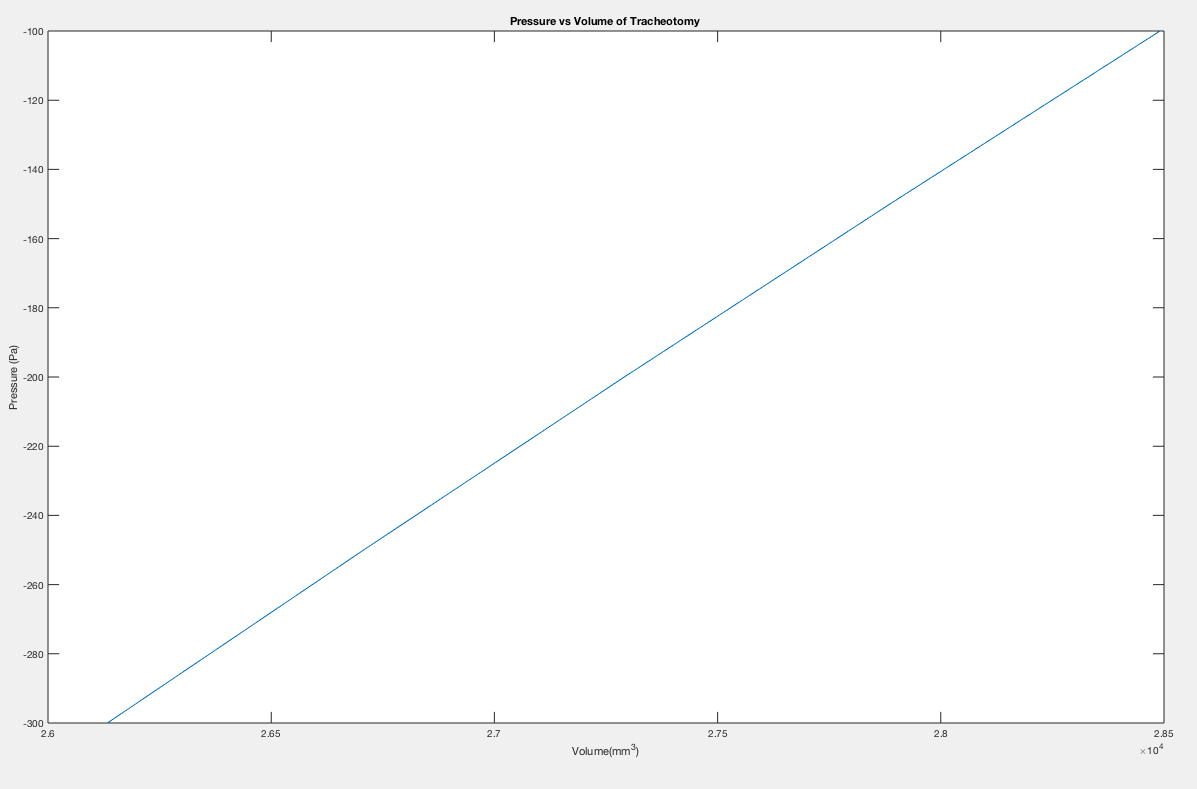
Figure 2:
Pressure vs Volume of Tracheomalacia
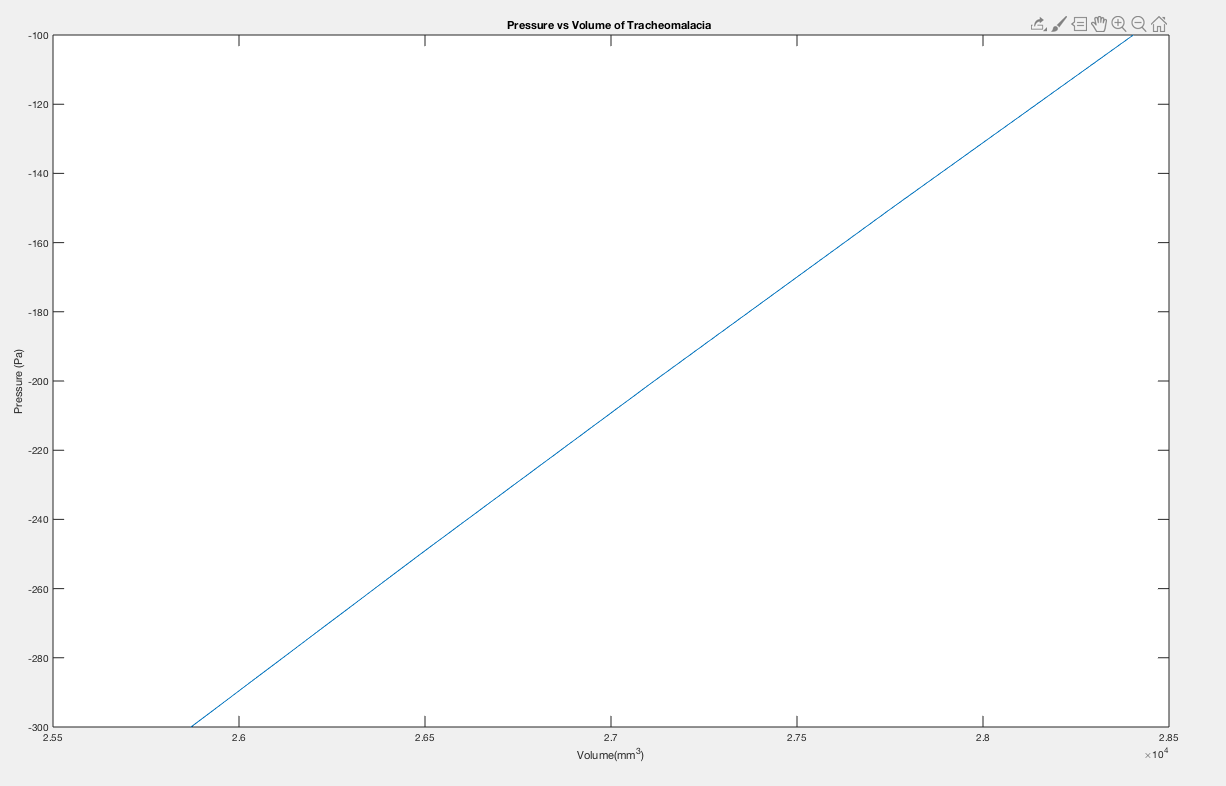
Figure 3:
Pressure vs Volume of Tracheotomy
The aim of this study was test the reliability of ANSYS simulated data to experimental data.The data showed an agreement with data presented by Costantino et al. for pre-term lambs. Costantino et al. reported normalized compliance of .013 and .053 cmH20 -1for an inflating and deflating trachea. Given that the simulated data produces values of .039, .045, and .0406 cmH20- 1 for normal trachea, tracheomalacia and tracheotomy, respectively, there is a reasonable agreement with experimental results. Although, Sofi et al. present data of on the effects of a tracheotomy on compliance, the value are not normalized and a direct comparison cannot be made. However, Sofi et al. report that a statistically insignificant change was observed for static compliance but a statistically significant change improvement in dynamic compliance. Since this simulation may be considered static and a small change was observed, the simulation seems to agree with the experimental correlation-although more simulation data is needed for statistical testing. Although, little data is available concerning tracheomalacia, an increase in compliance is expected and this is what was observed.
McNamara, V. M., and D. C. G. Crabbe. “Tracheomalacia.” Paediatric Respiratory Reviews, vol. 5, no. 2, June 2004, pp. 147–154. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=15135125&site=eds- live&scope=site
Paul De Leyn, Lieven Bedert, Marion Delcroix, Pieter Depuydt, Geert Lauwers, Youri Sokolov, Alain Van Meerhaeghe, Paul Van Schil, Tracheotomy: clinical review and guidelines, Journal of Cardio-Thoracic Surgery , Volume 32, Issue 3, September 2007, Pages 412–421, European
Boazak, Elizabeth M., and Debra T. Auguste. “Trachea Mechanics for Tissue Engineering Design.” ACS BIOMATERIALS SCIENCE & ENGINEERING, vol. 4, no. 4, pp. 1272– 1284. EBSCOhost, doi:10.1021/acsbiomaterials.7b00738. Accessed 19 Dec. 2020.
Sofi, Khalid, and Tariq Wani. “Effect of tracheostomy on pulmonary mechanics: An observational study.” Saudi journal of anaesthesia vol. 4,1 (2010): 2-5. doi:10.4103/1658-354X.62606